Systemic vs. Localized: The Scope of Corticosteroid Treatment
A deep dive into whether systemic or localized corticosteroid treatments are more effective for emergency asthma control.
Systemic vs. Localized: The Scope of Corticosteroid Treatment
Posted by Dr. Oliver Williams, reviewed by Dr. Helena Rodriguez | 2024-Apr-02
Asthma, a chronic respiratory condition characterized by airway inflammation and constriction, is a persistent challenge for healthcare providers and patients alike. When an asthma attack strikes, swift and effective treatment is crucial to alleviate symptoms and prevent potentially life-threatening complications. At the forefront of this emergency care are corticosteroids, a class of medications known for their potent anti-inflammatory properties.
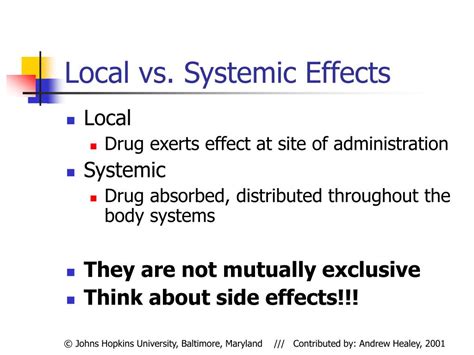
The debate surrounding the optimal use of corticosteroids in asthma management often centers on the choice between systemic and localized treatment approaches. Systemic corticosteroids, administered orally or intravenously, work to reduce inflammation throughout the body, while localized treatments, such as inhaled or nebulized corticosteroids, target the airway directly.
Proponents of systemic corticosteroids argue that this approach offers a more comprehensive and immediate response, as the medication is rapidly distributed to all affected areas. This can be particularly beneficial during acute asthma exacerbations, where a swift reduction in airway obstruction and symptom relief is crucial. Studies have shown that systemic corticosteroids can significantly improve lung function and reduce the risk of hospitalization in such cases.
On the other hand, advocates of localized corticosteroid therapy highlight the potential for reduced side effects, as the medication is delivered directly to the site of inflammation in the lungs, rather than being dispersed throughout the body. Inhaled or nebulized corticosteroids have been associated with a lower incidence of systemic adverse effects, such as adrenal suppression or metabolic disturbances, which can be a concern with prolonged systemic use.
Furthermore, the targeted nature of localized corticosteroid treatment may be particularly advantageous for managing chronic asthma, where the goal is to maintain long-term control and minimize the need for rescue medications. By delivering the medication directly to the airways, localized treatments can effectively reduce airway inflammation and hyperresponsiveness without the potential for systemic complications.
Ultimately, the decision between systemic and localized corticosteroid treatment in asthma management should be guided by the individual patient's needs, the severity of their condition, and the specific clinical scenario. Healthcare providers must carefully weigh the potential benefits and risks of each approach, taking into account factors such as the patient's age, comorbidities, and response to previous treatments.
As research continues to evolve, the role of corticosteroids in asthma care may further be refined, leading to more personalized and effective treatment strategies. The ongoing exploration of this topic highlights the importance of continuous collaboration between healthcare professionals, researchers, and patients in the pursuit of optimal asthma management.
So, the question remains: when faced with an asthma emergency, should clinicians opt for systemic or localized corticosteroid treatment? The answer, it seems, lies in a careful consideration of the individual patient's needs and the nuances of their condition.
User comments
More Topics to Explore
Cortisone to the Rescue? Debating Its Use in Asthma Flares
This thread invites opinions and experiences on the effectiveness and side effects of cortisone injections during severe asthma episodes.
Inhalers vs. Oral Steroids: Which Works Faster in a Pinch?
A discussion on the comparative speed and efficacy of inhalers versus oral steroids for immediate asthma relief.
Are Long-term Corticosteroids Worth the Risk for Chronic Sufferers?
This thread explores the balance between the benefits and potential risks of long-term corticosteroid therapy for chronic asthma.
Surviving the Night: Emergency Corticosteroid Protocols
Share and learn about emergency corticosteroid protocols specifically for night-time asthma attacks.
Nebulizer Treatments: Corticosteroids at Home?
A discussion on the feasibility and safety of administering corticosteroid nebulizer treatments at home for severe asthma cases.
Post-Emergency Care: Preventing Relapse with Corticosteroids?
This thread examines if corticosteroids can effectively prevent relapses after an asthma emergency.
Interactions Alert: Corticosteroids and Other Meds in Asthma Emergencies
A discussion focusing on the potential interactions between corticosteroids and other medications during asthma emergencies.
Side Effects Showdown: Weighing Corticosteroid Pros and Cons
Weigh in on the side effects of corticosteroids and how they balance against their benefits in emergency asthma care.
Pediatric Asthma: Safeguarding Kids with Emergency Corticosteroids
A crucial conversation on the use of corticosteroids in emergency care for children with asthma.
Speedy Relief? Timing of Corticosteroid Administration
Explore how the timing of corticosteroid administration can impact its effectiveness in treating asthma attacks.
Corticosteroids Inhalers: A Bridge Over Troubled Breathing?
Discuss the role of corticosteroid inhalers in ongoing asthma management and emergency situations.
Alternative Routes: Injection vs. Oral Corticosteroids in Crisis
Compare experiences with injectable versus oral corticosteroids during an asthma crisis to determine the most effective approach.
Battling Inflammation: Corticosteroids as the First Line of Defense?
This thread questions whether corticosteroids should be the first line of defense in controlling inflammation during an asthma attack.
Breathlessness and Anxiety: Can Corticosteroids Help Both?
Explore whether corticosteroids can address both the physical symptoms of an asthma attack and its accompanying anxiety.